

With modern surgical techniques, a greater than 90% primary anatomic success rate can be expected following retinal detachment repair. However, one year after retinal reattachment, he was noted to have an inferior tractional retinal detachment in the right eye with areas of subretinal fibrosis. Fundus photography performed during a follow-up visit revealed a flat retina in both eyes, though there was residual fibrosis in the right eye (Figure (Figure3). His IOP remained stable over the next year on the same medication regimen. There was complete regression of the rubeosis. At two months after AC washout and three months after presentation, pars plana vitrectomy, membrane peel, retinotomy with aspiration of subretinal blood, endolaser retinopexy, inferior iridotomy, air/fluid exchange and retinal reattachment with silicone oil were performed.įollowing surgery, his vision improved to counting fingers vision in the right eye at five metres, with IOP of 12 to 17 mmHg (right eye) on two antiglaucoma medications. Given the good appearance of the retina and because he had recovered LP vision, we decided to see if vision would improve further by repairing the detachment. His retina was noted to be normal in color and not necrotic or cystic. Over eight weeks, his IOP gradually decreased to 15 mmHg (right eye) on four antiglaucoma medications, and his visual acuity improved from NLP to LP. Over the next three weeks, he had two doses of 1.25 mg/0.05 ml intravitreal bevacizumab two weeks apart to treat his neovascularization. AC washout was performed, and during surgery he was noted to have NVG with 360° rubeosis iridis, and vitreous hemorrhage with ghost cells. Over the following two weeks, his IOP fluctuated between 36 to 50 mmHg (right eye), with no resolution of the hyphema or pain. Immediate AC paracentesis to relieve pain and pressure reduced the IOP to 38 mmHg. Ultrasonography (right eye) at presentation, indicating low retinal detachment and vitreous hemorrhage. Ultrasound of the right eye revealed low-lying retinal detachment with vitreous hemorrhage (Figure (Figure2 2). Dilated fundus examination of his left eye revealed two areas of laser retinopexy surrounding lattice degeneration at 1:00 and 3:00 o'clock. Intraocular pressure (IOP) by Goldmann applanation tonometry was 60 mmHg (right eye) and 10 mmHg (left eye). He had an unremarkable examination of his left eye, with early nuclear sclerosis. Slit lamp examination revealed right eye nasal and temporal band keratopathy, mild corneal edema, total hyphema and no posterior view given the hyphema (Figure (Figure1).
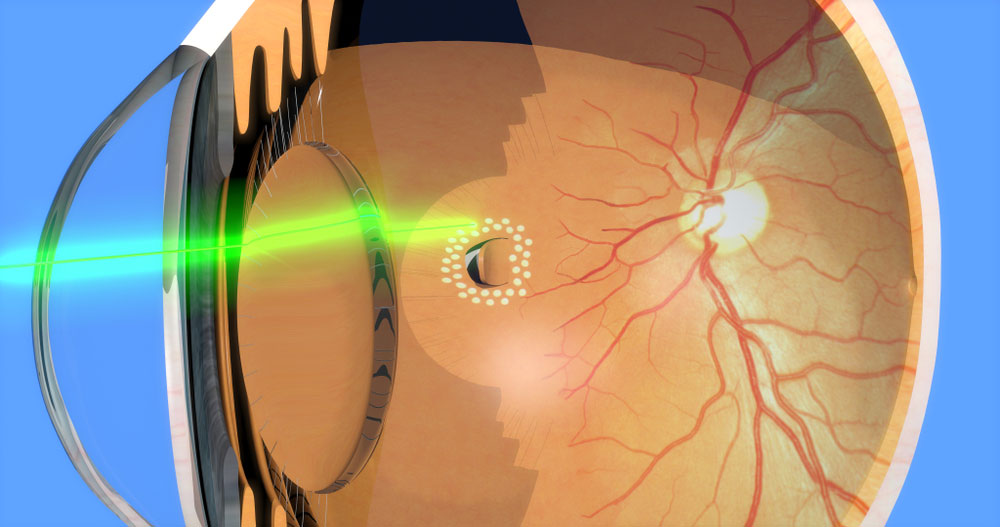

External examination showed ptosis and exotropia in his right eye. On examination, his visual acuity was NLP (right eye) and 20/20 (left eye). He had a history of diabetes mellitus, quadruple cardiac bypass surgery, and defribillator implantation. At age 39, he had laser retinopexy in his left eye for lattice degeneration. His best corrected visual acuity post lensectomy was light perception (LP), with a persistent retinal detachment. He subsequently developed a cataract in his right eye, for which he underwent cosmetic lensectomy at age 25. He had had a traumatic retinal detachment of the right eye (55 years ago) after being struck in the eye with a stone. We report the case of a patient with total hyphema, NVG, long-standing retinal detachment and no light perception (NLP) vision, who regained counting fingers (CF) vision with complete regression of the neovascularization following anterior chamber (AC) washout, intravitreal bevacizumab, and two retinal reattachment surgeries.Ī 63-year-old Caucasian man presented to our facility with a four-week history of pain and redness in his right eye. Retinal ischemia and hypoxia initiate the release of angiogenesis factors, with consequent development of new vessels. NVG represents one of the most severe forms of secondary glaucoma, caused by a number of ocular and systemic conditions. Ĭhronic retinal detachment is a cause of rubeosis iridis and neovascularization of the anterior chamber angle with subsequent neovascular glaucoma (NVG). Long-standing retinal detachments (over one year) with poor visual acuity are typically associated with cystic degeneration of the macula and retina, loss of pigment from the underlying retinal pigment epithelium, proliferative vitreoretinopathy, and poor visual outcome after retinal reattachment surgery.


 0 kommentar(er)
0 kommentar(er)
